MTSS (medial tibial stress syndrome) or ‘shin splints’ is the name often given to exercise-induced pain in the shin bone (the tibia) most likely associated with repetitive stress to the muscles, tendons, and tissues that attach to the shin bone.
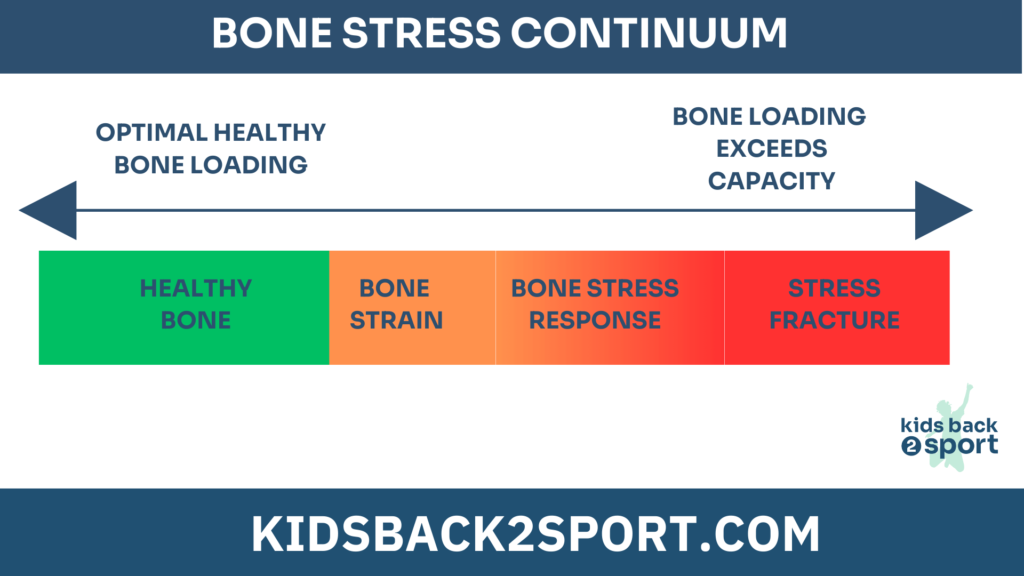
They are prevalent within an adolescent population, particularly at certain times of the year. It’s important to be mindful that MTSS is a bony injury, and the severity of the condition lies within a continuum from localised inflammation with swelling through to changes in the bone itself resulting in some instances, a hairline fracture.
Therefore, treatment should be guided in accordance with a bone stress injury and shin pain is not something we should accept amongst this population.
Where is the pain?
Typically, the athlete will present with pain and tenderness along the inside of the shin bone during or after running or doing exercise. However, not all “shin splints” are equal. It is worth knowing that pain felt over the front of the shin bone is regarded as more high risk as the shape of the bone creates more tension on the injury site and poor blood supply to this region of the tibial bone makes healing slower. Conversely, pain felt on the inside of the lower shin bone, closer to the back of the bone is considered “low risk” because given the right management, it has the potential to heal quicker.

Why may this happen?
A spike in activities that cause an increase in demand of the muscles that plantarflex the ankle is the main cause for MTSS and this can occur for several reasons:
• Increased amount or intensity of sprinting (athletics)
• Increased amount or intensity of jumping (netball)
• Increased amount or intensity of change of direction (tennis)
• Increased amount or intensity of running volume on hard surfaces (hockey)
• A change in a usual training plan
Further considerations and risk factors include:
Maturation status: Where the individual sits within their adolescent development matters. Children go through a more rapid growth spurt termed peak height velocity (PHV) in girls around the aged of 11 and in boys around the age of 13, but this timing varies between individuals. The faster the growth spurt, the greater the resulting stress on the surrounding tissues. There are metabolic and hormonal considerations at play. Rapid elongation of the bone lowers the bone density temporarily making it more susceptible to bone stress injuries. Increases in bone length creates longer levers creates greater tension on surrounding muscles and may result in a period of adolescent awkwardness changing their coordination and biomechanics.
Muscle strength deficits: A lack of capacity in the ankle plantar flexors and hip extensor muscles means an individual will fatigue sooner and have subsequent excessive strain on the attachment of the muscle to the bone sooner.
Training errors: Understanding that it is not just too much too soon, but also how hard the training is. Intensity within training load matters.
Acute to chronic workload ratio: The “chronic” load equates to the training completed in the last 3-4 weeks that has prepared the athlete for the current or “acute” training load. If the athlete has not completed sufficient training volume or at a high enough intensity for the demands of the current week, the acute to chronic workload ratio may climb above the athlete’s current capacity and injury may result. The ability to recover and allow bone to remodel suffers within dense competition blocks where the session frequency may not have changed, but the session intensity may well have as the athlete applies maximal effort.
Foot shape: Historically there has been evidence suggesting an increased navicular drop (a bone on the inside of the arch) may be associated with MTSS, likely due to excessive internal rotation of the tibia which can increase the degree of pronation in the foot.
Mechanics: running style has been associated with injury risk. A narrow base of gait or a criss cross gait can create increased velocity of pronation causing increased tibial stress.
Nutrition: Vitamin D and calcium help bone regeneration. Low levels of iron and calcium within the diet can affect bone health. There are some athletes who cannot absorb the nutrients in food due to food allergies and digestive disorders. Another factor relating to bone health is the presence of low energy availability. This occurs when there is a mismatch between what an athlete consumes relative to what they use during their sporting activities. If they are in a negative energy balance where they fail to eat enough for what they do, it can impact both wellness and bone health placing the athlete more at risk of bone stress injuries.
What can we do about it?
The priorities within rehabilitation are:
- Educate the athlete around the risk factors that might have led to the injury.
- Address any deficits in energy availability.
- Supplement Vitamin D and increase calcium and iron within the diet where necessary.
- Activity modification: This may mean reducing, and often completely avoiding, any high intensity or high impact activity for a period to allow adequate recovery to enable healing. Switching to other low impact exercises such as cycling or swimming can help to maintain fitness. The longer you have had symptoms, the longer it may take to settle.
- Strengthen the ankle plantar flexor and hip and trunk muscles.
- Lengthen the calf muscle complex where appropriate.
It is important not to take pain medication to enable the athlete to continue playing sport as this may mask symptoms and result in more a extensive injury that takes longer to heal.
How do I know when I can run again?
To test if you are ready to try resuming running, try hopping on the spot. If it hurts to hop on the spot, you are not ready to run. Running is in effect a series of hops, so this is a good way to assess not only readiness to train, but also a useful tool to check how well you reacted to increasing activity level. If you have started to add back activities, test your response the next day by hopping on the spot and assess if it is worse of better than in previous days.
Once the bone has had time to adapt, recover and become stronger, a gradated multi directional plyometric programme and a phased return to running/training can begin. It is important not to return at the same level as preinjury straight away or the inflammation and stress on the bone will quickly recur. The rate of progression back to running will depend on how long you have been out of action.
Do I need an x-ray or scan?
If the pain does not settle with rest, or the pain is present at rest, it is worth making an appointment to see a health professional who has experience of seeing sporty children. In some instances, an MRI scan may help to confirm a diagnosis and to highlight the degree of injury and establish if there is a fracture present which may require a period of time in a fracture walking boot to allow complete healing.
How do I stop it recurring?
The highest risk factor for an injury like this is having had one before. Therefore, it makes sense to make a positive change. This should start with managing and tracking training load ensuring no sudden spikes in volume or intensity especially at the start of a season or when seasons overlap. Maintaining calf strength and length makes sense along with an ongoing sport plyometric strengthening programme. Running alone does not optimise tibial loading, however, plyometrics and high weight low repetition lower limb strengthening do, which creates positive stress and subsequent adaptations to surrounding tissues of the tibia.

Glen Lewis / Chartered Physiotherapist May 2024
Instagram : physioglen
X : physio_glen
Contact Glen:
https://www.butlerphysiotherapy.co.uk/
References:
https://pubmed.ncbi.nlm.nih.gov/33962529/ https://pubmed.ncbi.nlm.nih.gov/30066165/
https://pubmed.ncbi.nlm.nih.gov/28179260/
https://radiopaedia.org/cases/fredericson-mri-classification-of-medial-tibial-stress-syndrome?lan g=gb